This is part of Six Months In, a Slate series reflecting on half a year of coronavirus lockdown in America.
On the morning of Tuesday, March 10, Skagit County Public Health declared a public health emergency. Officials in the county, about 100 miles north of Seattle, had identified its first confirmed case of COVID-19—a woman in her 40s who appeared to have acquired the virus from community transmission, not travel. To slow the virus’s spread, the health department recommended residents maintain physical distance from one another and limit gatherings to 10 people.
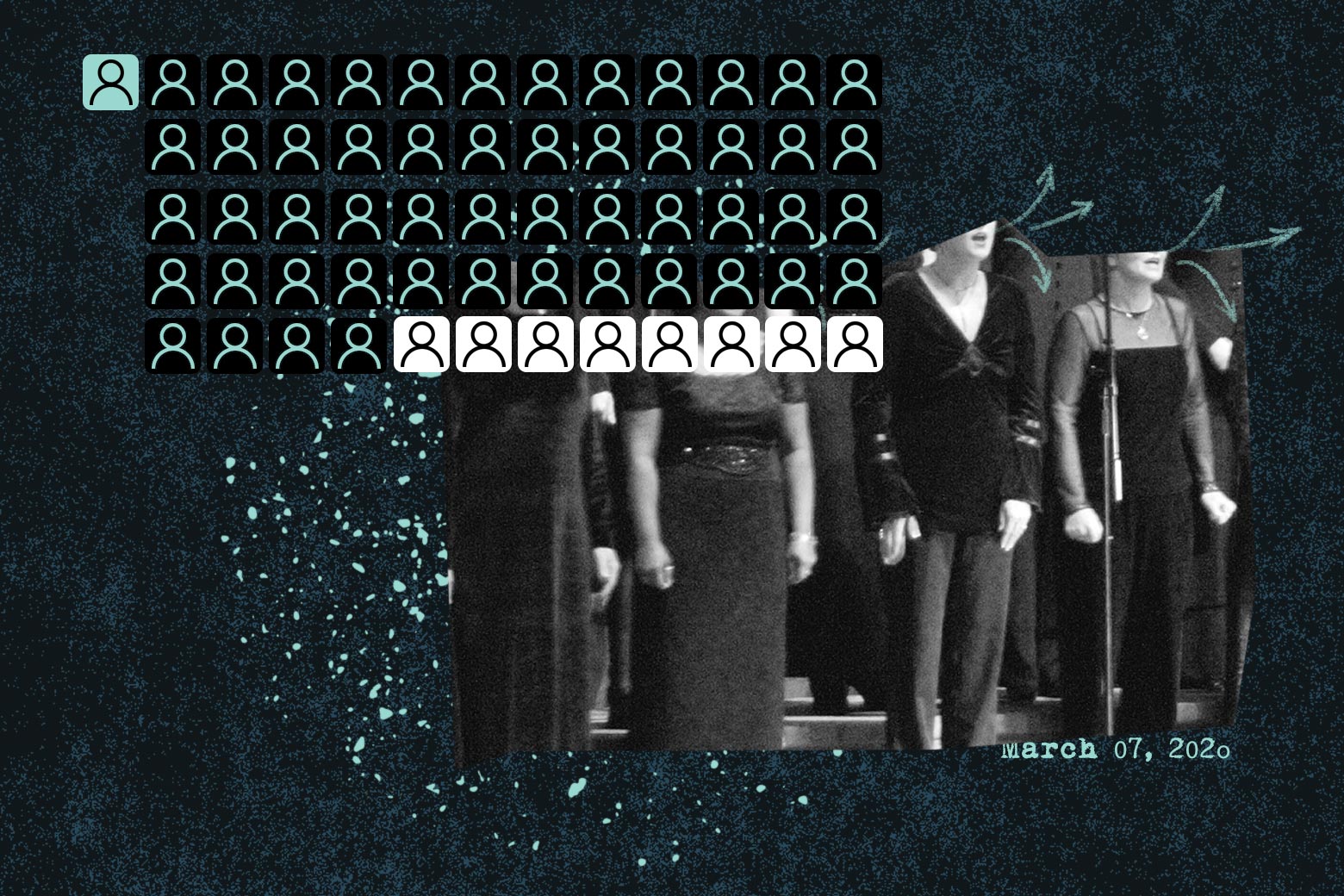
That evening, 61 members of the Skagit Valley Chorale met for their regular practice. They avoided their customary hugs and handshakes. For 2½ hours, the members, many of them older adults, sang together in Mount Vernon Presbyterian Church. By the end of the week, six people felt sick. In all, 53 attendees had confirmed or suspected cases of the coronavirus. By the end of the month, two Skagit Valley Chorale members had died.
The superspreader event made Skagit Valley, otherwise known for its technicolored tulip farms, the focal point of endless international interest. (Members of the choir board declined to comment for this story, citing a desire to focus on the future.) The case went on to inflame a life-or-death debate about how to form scientific consensus in a pandemic—one that remains unresolved six months into lockdown in the United States.
On March 17, a week after the practice, the Skagit Valley Chorale appointed a member to contact the health department and inform it of a possible COVID-19 outbreak. Epidemiologist Lea Hamner was tasked with piecing together the definitive account of the disease’s spread among the singers. Through multiple interviews with attendees, Hamner and her team determined that there was likely one infected person at the practice, who’d begun showing coldlike symptoms on March 7 and subsequently spread the disease to everyone else. The report, which was published by the U.S. Centers for Disease Control and Prevention on May 15, concluded that there were multiple opportunities for the virus to be transmitted through close contact or contaminated surfaces. It left open, but did not endorse, the possibility the virus was in the air.
By the time the full story emerged, the debate about how COVID-19 spreads—and what that meant for mitigation efforts—had been underway for months. In February, the World Health Organization announced that COVID-19 was transmitted via heavy droplets that spread in close contact or fell on surfaces like door handles and kitchen countertops—hence the predominant advice to wash your hands. Airborne spread was “not believed to be a major driver of transmission based on available evidence,” the report stated. At the time, the CDC was focused on the dangers of close personal contact, with investigations into surface and aerosol transmission still on the horizon. But environmental chemists and engineers who study aerosols were already questioning these assumptions.
Along with new data at the time on the virus’s potential for asymptomatic spread—cases when infected people are less likely to spew heavy droplets through coughing—the report out of Skagit Valley further intensified the transmission discourse: If COVID-19 could spread so thoroughly and quickly through a choir, did that mean the coronavirus was airborne? And if the primary route for the disease’s spread was through the air, had our initial response been woefully misguided?
For researchers like Linsey Marr, a professor of civil and environmental engineering at Virginia Tech, the answer was clear: The coronavirus is airborne, and the superspreader choir proved it. Over the summer, scientific consensus has slowly shifted to understand that the virus could be set afloat by speech—or song—and remain in the air long enough to infect those who inhale it. But Marr had always suspected COVID-19 might move this way, based on previous research suggesting that other coronaviruses, SARS and MERS, were also transmitted through the air. It was the Skagit Valley data “that really convinced me that it was spreading through the air, because it’s really hard to explain those numbers—53 infected out of 61—any other way,” she said.
Jose-Luis Jimenez, a chemist at the University of Colorado Boulder, felt similarly. In June, he and his colleagues published a preprint paper on the Skagit Valley Chorale. They argued that if the health department was correct and one unwittingly COVID-positive person transmitted the disease to everyone else, it must have been from the air and not through surface contact. As they describe in a revised version of the paper, there was limited physical contact among participants, the practice was at half capacity, hand sanitizer was dispensed at the door, and the COVID-positive person did not help with arranging chairs or distributing snacks. Using a box model (a system of calculating how particles spread in a closed environment) and the Wells-Riley equation (a formula for determining the risk of infection, originally developed to show that measles could be airborne), Jimenez and his colleagues argued the outbreak had to have spread through the aerosols, perhaps propelled by the singing itself.
That view still isn’t universal. Even back in March, a Skagit Valley health department representative told the Los Angeles Times that the virus must be airborne to have infected so many choir members so quickly. But when I spoke to Hamner, the epidemiologist who led the subsequent investigation, she remained agnostic. “Plenty of researchers have approached us trying to say this is an airborne transmission event,” she told me. “We’re not saying it’s not. But we couldn’t rule anything out.” She added that contaminated surface “transmission seems unlikely, based on additional evidence, but at that time, we weren’t willing to rule that out either. It was a perfect storm, frankly.”
Once agencies like the WHO established the position that COVID-19 was spread primarily through heavy droplets, it was a tall order to change it. “They’ll die defending their view,” one anonymous WHO consultant told the New York Times in July. Even now, “the burden of proof is much higher for aerosols than for any other route, and yet we have more evidence for aerosols in this case than for any other route,” Marr told me.
But what may seem like a disagreement about droplets is actually just another in a series of long-standing issues in international health illuminated by the pandemic. From an organizational standpoint, the WHO aims to avoid burdensome recommendations to member nations, which vary dramatically in the resources they can commit to fighting a virus. To the public, airborne simply means something can move through the air, but for the medical establishment, it’s a loaded word, Marr explained. If an organization like WHO were to classify COVID-19 as airborne like the measles and tuberculosis, then health care organizations would have to take specific, and often onerous, precautions, including investing in N95 respirators (instead of simple surgical masks) and ventilation systems that keep particles contained.
These definitional issues speak to deeper rifts in the scientific community: Medical researchers, Jimenez argued, are skeptical of the more theoretical tactics that aerosol scientists use, including mathematical modeling. For public health purposes, proving surface transmission requires finding a live virus on an elevator button or handrail, while proving aerosol transmission requires identifying clear cases of long-distance disease transmission.
Aerosol scientists say they are also up against a long-standing historical bias against aerosols in medical research. One factor is their invisibility: Bacterial cultures, for example, can be cultivated and observed under a microscope, but sampling aerosols is technologically intensive and difficult to accomplish even in lab environments. Many also believe science has simply moved on: For centuries, the dominant “miasma theory” held that disease was the direct result of bad air. When germ theory dethroned miasma theory, airborne illnesses as a whole were second-guessed. The result is that early COVID-19 guidelines prioritized hand-washing and heavy droplets, initially to the exclusion of mask-wearing and aerosols.
Some aerosol scientists remain cautiously optimistic that this schism can be resolved as the pandemic continues to rage. After 239 experts wrote an open letter to the WHO laying out the evidence for airborne transmission, the organization capitulated—partially. On July 9, the agency released an updated scientific brief conceding that the coronavirus could linger in the air in crowded indoor spaces. The WHO has continued to emphasize “that droplet and fomite transmission could also explain human-to-human transmission.” But, Marr said, “I’ve seen more movement [on aerosols] in the last five months than in the last 12 years.”
The aerosol dilemma is a microcosm of countless other pandemic debates happening in real time. As public health agencies aim to share the latest information, even when there is no scientific consensus, they inevitably promote some ideas that prove to be wrong, and others that stand up. The goal is to save lives, but the messy process can end up undermining public trust. As the science—and the stories we tell ourselves about it—continues to evolve, so too will our behaviors. For now, whether it’s aerosols or heavy droplets that scare you most, singing in a large group is probably a bad idea.